Application Focus - Electroporation Mediated Creation of a Dendritic Cell-Based Cancer Vaccine
By George Kamphaus, Ph. D.
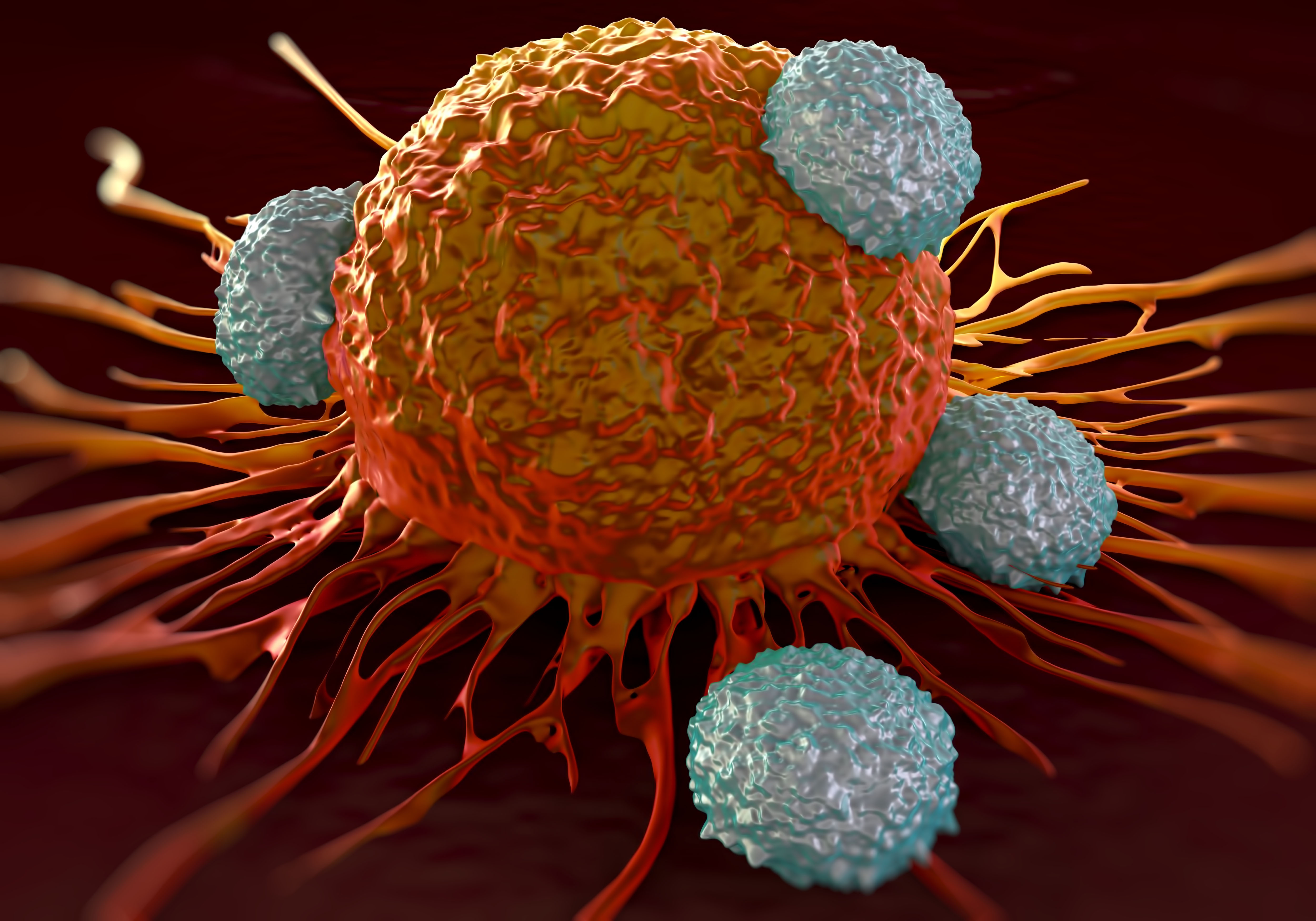
This blog describes a new method for creating vaccines against tumors. Shadi-Yunger, et al.1 have created a novel MHC-II platform by generating a chimeric invariant chain, in which the semi-peptide CLIP is replaced with essentially any tumor specific peptide. This hybrid MHC-II chain facilitates the activation of CD4+ T-cells when expressed in dendritic cells (DCs). In this particular study, the researchers attempted to create an anti-melanoma vaccine by inserting different melanoma-associated antigens (MAAs) mRNA sequences into the MHC-II hybrid construct. The hybrid MHC-II chain is then combined with another novel MHC-I light chain chimera created by the same group. The MHC-I construct converts the light chain into an integral membrane protein by linking an antigenic peptide (in this case an MAA peptide sequence) at the extracellular N-terminus and coupling to either the membrane anchoring Kb sequence or the intracellular TLR4 signaling domain at the C-terminus. In multiple experiments, different MAA sequences were inserted into the hybrid constructs and mRNAs coding both the hybrid MHC-I and MHC-II were transfected into murine bone marrow derived dendritic cells (BMDCs) by electroporation using the BTX ECM 830 generator. These transfected BMDCs were then injected into mice bearing tumors from Ret melanoma cells, to assess the anti-tumor activity and T-cell activation stimulated by these modified DCs.
A brief description of the electroporation protocol (Please see Shadi-Yunger et al.1 for method details.)
- BDMCs isolated from femurs and tibiae of 4 to 5 weeks old C57BJ/6 female mice were cultured for 10 days. On the day of transfection cells were washed two times with Opti-MEM (GibcoBRL) and resuspended into Opti-MEM medium containing 10 to 20 g of transcribed mRNA.
- Add mixture to electroporation cuvette (for example, Cuvettes Plus, 2 mm gap, BTX).
- Electroporation: 1 pulse (square wave) at 400 V, 0.9 ms pulse duration.
- Collect cells from the cuvette and resuspend in 5 ml of pre-warmed media and place into 50 ml tube for further incubation.
Selecting MAAs for the anti-tumor vaccine
Since prior studies had shown spontaneous anti-melanoma immune responses could be directed against melanocyte differentiation antigens such as gp100, tyrosinase (Tyr) and tyrosinase related proteins 1 and 2 (TRP-1 and TRP-2), these proteins have been studied to find peptides or fragments that could enhance immune anti-tumor responses. Prior to this study, the authors had tested the anti-tumor activity of two such peptides as part of chimeric polypeptide sequences, gp10025-33 and TRP2180-188. By further expanding their search using SYFPEITHI prediction software, they were able to find several other peptides for study as MHC-I MAAs. The two chosen for hybridization in the MHC-I constructs this study were TRP1455-463 (designated E120 in the figures) and Tyr360-368 (called E124) both of which bind, or are predicted to bind to H-2Db
Two different MAA peptides were chosen for the creation of MHC-II chimeric proteins. The first was TRP-1111-128 (designated E122) which was previously shown to confer immune response, and Tyr99-117 (aka E130) which was predicted to induce an immune response by the IEDB prediction tool.
Characterization and functional analysis of transfected BMDCs
- Cells were assessed for expression of MHC-I chimeric constructs by flow cytometry 6 hrs after electroporation using anti-β2m antibody.
- MHC-II constructs could not be assessed using commercial antibodies, so instead surface expression was determined by the ability to induce proliferation in T-cells from mice immunized with the corresponding MAA peptide. Proliferation was assessed by in vitro H3-thymidine uptake assays. Two different hybrid MAA-CLIP MHC-II constructs were able to stimulate CD4+ T-cell proliferation with similar kinetics as the corresponding peptide-loaded BMDCs.
- BMDCs transfected with the hybrid MHC-I constructs alone were able to induce targeted cell killing by T-cells in both in vivo and in vitro CTL experiments.
In vivo anti-tumor vaccine studies
Once the authors concluded that the chimeric MHC-I and MHC-II proteins were expressed and functional when the mRNA constructs were transfected into BMDCs, they performed several in vivo studies in Ret melanoma injected mouse tumor models. The results, summarized below, indicate that a melanoma vaccine will likely require a combination approach; multiple antigens and induction of both MHC-I and MHC-II responses. Furthermore, it appears that CD4+ T-cells are important mediators of anti-tumor response.
- BMDCs transfected with a combination of E120-MHC-I and E124-MHC-I constructs were injected 3 times at weekly intervals (5 x 105 cells/mouse/injection) showed significant inhibition of tumor growth and increased survival (number of days until 8mm tumor size) compared to control and compared to E124 construct-BMDCs alone.
- BMDCs transfected with E120-MHC-I alone on the same schedule, also showed inhibition of tumor growth and some enhanced survival, but not as great as the dual transfected group.
- In similar Ret melanoma tumor models, the two TRP1 peptide sequences, E120 and E122, were cloned into separate MHC-I and MHC-II chimera constructs and transfected into BMDCs. When both mRNAs were transfected, BMDC vaccination resulted in significant tumor inhibition and prevented all the mice in that group (n = 8) from reaching the criteria for termination. This result was significantly better than either construct alone.
- In addition, when the two Tyr peptides, E124 and E130, were introduced into the MHC-I and MHC-II chimera constructs respectively and transfected into BMDCs. Just as before, BMDCs with Tyr peptides in both the MHC-I and MHC-II format showed prolonged survival and slower tumor growth than the groups vaccinated with only E124-MHC-I or E130-MHC-II containing BMDCs alone.
3) Immunization with the chimeric MHC-MAA constructs generates CTLs, Th1 and Th2 immune responses.
- To understand the mechanism of tumor growth inhibition observed in the Ret melanoma model the researchers removed the spleens of the treated mice to characterize the immune cell populations.
- Of the groups treated with BMDCs transfected with MHC-I only constructs (E120-TRP1, E124-Tyr or both together) only the E120 alone group showed a statistically significant increase in the % of IFNγ+, TNFα+ and IFNγ+/TNFα+ (double positive) CD8+ T-cells. The other treatment groups showed some elevated levels of these CD8+ cells, but due to low numbers of treated mice (n = 3) these were not significant.
- When BMDCs transfected with TRP1 MAA chimeras as MHC-I and MHC-II constructs alone or in combination (E120-TRP1, E122-TRP or both together) were used a treatment, both the E120 group and the E120+E122 groups showed a statistically significant increase in the % of IFNγ+ CD8+ cells. E122 by itself had little to no effect on the CD8+ cell populations measured. Both E120 and E120+E122 treated groups showed a mild but not statistically significant increase in the % of TNFα+ and IFNγ+/TNFα+ (double positive) CD8+ T-cells.
- When the researchers looked at CD4+ T-cell populations the trends were similar to CD8+ results. However, more of the treatment groups showed statistically significant increases above control. Importantly, the MHC-II chimeric construct E122 in BMDCs showed statistically significant increases in the % of IFNγ+, TNFα+ and IFNγ+/TNFα+ (double positive) CD4+ T-cells. This seems to indicate that MHC-II is a better mediator of CD4+ cell response than of the CD8+ T-cell response.
- Another observation was that the increases in the percentages of cytokine expressing CD4 and CD8 T-cells did not match proportionally to the tumor growth inhibition. That is, the combination transfected BMDC treated groups that showed increased survival and slower tumor growth were not the groups with the greatest % increase in of IFNγ+, TNFα+ and IFNγ+/TNFα+ (double positive) CD4+ or CD8+ T-cells.
- When the authors looked at Th2 populations (CD4+/IL-4+ ) all of the combination treatments, E120+E124 in MHC-I constructs, E120-MHC-I + E122-MHC-II and E124-MHC-I + E130-MHC-II appeared to have increased % of Th2 cells compared to the single constructs alone. Again, due to group sizes being small, only the TRP1 MAAs in the MHC-I + MHC-II combination (E120+E122) showed a significant difference from control.
Reference:
1. Sharbi-Yunger, A., et al. (2019). A universal anti-cancer vaccine: Chimeric invariant chain potentiates the inhibition of melanoma progression and the improvement of survival. International Journal of Cancer, 144, 909-921.
Buy an ECM 830 Electroporation System, get a free BTXpress High Performance Electroporation Buffer—Click here for promotion details!



 800-272-2775
800-272-2775
